Rejuvenation of the Lower Eyelid Complex
Stephen W. Perkins, M.D.1 and Rami K. Batniji, M.D.1
ABSTRACT
Blepharoplasty is one of the most common cosmetic surgeries performed on the male patient. Whereas in the past the male patient would present later in life for eyelid surgery to address functional issues, he now presents earlier in life with an interest in aesthetic improvement as the primary motivating factor. This article reviews the approach of the senior author (SWP) to rejuvenation of the lower eyelid complex. Specifically, we discuss the indications for and techniques of the transcutaneous and transconjunctival approaches for blepharoplasty. As well, adjunctive procedures for rejuvenation of the lower eyelid complex, including fat transposition, lateral canthoplasty, and skin resurfacing, are reviewed.
KEYWORDS: Blepharoplasty, fat transposition, canthoplasty, skin resurfacing
According to a survey of members of the American Academy of Facial Plastic and Reconstructive Surgery, blepharoplasty was the third most common cosmetic surgical procedure performed on the male patient in 2004, following hair restoration and rhinoplasty. These findings were corroborated by a similar survey of the American Society of Plastic Surgeons. Previously, a functional defect was the initial motivation for the male patient to seek surgery of the upper eyelids.
Also, the male patient tended to present later in life compared with the female patient. However, now it is not uncommon for the male patient to present both earlier in life and with an interest in aesthetic improvement as the primary motivating factor. Specifically, the male patient wishes to address the ”tired” look associated with age-related changes to the lower eyelid. This desire may stem from pressure experienced in the workplace to appear more energetic and vibrant compared with
younger colleagues. In addition, the patient’s significant other may encourage the patient to seek out consultation and accompany the patient during the initial visit to the facial plastic surgeon. This article reviews the approach of the senior author (SWP) to rejuvenation of the lower eyelid complex in the male patient.
ANATOMY OF THE LOWER EYELID COMPLEX
A thorough understanding of the lower eyelid complex anatomy is essential to both proper diagnosis and surgical
planning. The lower eyelid complex is composed of three lamellae.1 The anterior lamella consists of skin and pretarsal orbicularis oculi muscle. The middle lamella contains the orbital septum, which is an extension of the periosteum of the orbital rim. The posterior lamella consists of the inferior retractor muscles, tarsus, and conjunctiva. Orbital fat is located posterior to the orbital septum and is compartmentalized into lateral, central, and medial pockets of the lower eyelid; the inferior oblique muscle divides the middle fat pocket from the lateral fat pocket.
THE AGING LOWER EYELID COMPLEX
The aging process of the lower eyelid complex includes progressive loss of organization of elastic fibers and collagen, leading to dermatochalasis (loss of skin elasticity and subsequent excess laxity of lower eyelid skin).2 In addition, the orbital septum weakens with age, leading to steatoblepharon (pseudoherniation of orbital fat).3
Orbicularis oculi muscle hypertrophy is also associated with age-related changes of the lower eyelid complex.4 It is not uncommon for the male patient to present with festoons, which are folds of orbicularis oculi muscle in the lower eyelid that hang in a hammock-like fashion from the medial to lateral canthi; festoons may contain protruding orbital fat. Malar mounds refer to skin and fat that bulge from the malar prominence and are an agerelated change of the midface. Although the anatomic basis for malar mounds requires further delineation, potential causes include edema with subsequent fibrosis;
Mendelson et al believe that ptosis and volume loss of the midfacial soft tissue contribute to the formation of malar mounds.5 When ptosis and volume loss of the midfacial soft tissue occur in conjunction with pseudoherniation of orbital fat, a double convexity contour is noticeable and the nasojugal groove, or tear trough deformity, deepens.6
PREOPERATIVE ASSESSMENT
The preoperative assessment of the male patient seeking rejuvenation of the lower eyelid complex includes a history to evaluate for systemic disease processes, such as collagen vascular diseases and Graves’ disease, dry eye symptoms, and visual acuity changes. If any unusual history is gleaned from the preoperative assessment, it may be prudent to obtain an ophthalmologic evaluation prior to embarking upon surgical rejuvenation of the lower eyelid complex.
The physical examination should include assessment of visual acuity and extraocular movements for all patients. Schirmer’s test is indicated if there is concern about dry eye syndrome. Pseudoherniation of orbital fat can be demonstrated on the direction of the patient’s gaze. Gaze in the superior direction accentuates the lower central and medial fat pockets, whereas superior gaze in the contralateral direction accentuates the lateral pocket. Evaluation of both lower eyelid position and laxity is an essential component of the preoperative examination. The ideal position of the lower eyelid margin is at the inferior limbus.7 A snap test and lid distraction test are key components to the evaluation of lower eyelid laxity. A snap test is performed by grasping the lower eyelid and pulling it away from the globe. When the eyelid is released, the eyelid returns to its normal position quickly. However, in a patient with decreased lower eyelid tone, the eyelid returns back to its position more slowly. The lid distraction test is performed by grasping the lower eyelid with the thumb and index finger; movement of the lid margin greater than 10 mm demonstrates poor lid tone and a lidtightening procedure would be indicated.
LOWER LID BLEPHAROPLASTY
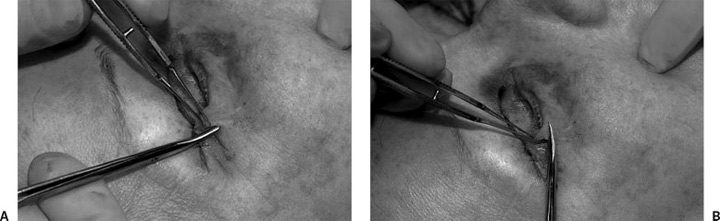
Blepharoplasty may be performed by a transconjunctival or transcutaneous approach. Among the transcutaneous approaches, the skin-muscle flap is the technique most commonly used by the senior author. The indications for this technique include true vertical excess of lower eyelid skin, orbicularis oculi muscle hypertrophy, and presence of pseudoherniation of orbital fat. The incision is 2 mm inferior to the lower lid margin and extends from the lower punctum medially to a position 6 mm lateral to the lateral canthus; lateral extension of the incision to this position minimizes rounding of the canthal angle. Following the skin incision, fine curved scissors are used to dissect through the orbicularis muscle at the lateral aspect of the incision (Fig. 1A). Then, blunt scissors are positioned posterior to the muscle at the lateral
aspect of the incision and, with spreading motions of the blunt scissors, the skin-muscle flap is effectively elevated off the orbital septum along an avascular plane to the level of the inferior orbital rim inferiorly and the incision superiorly (Fig. 1B). The subciliary incision is then completed using the scissors in a beveled manner to ensure the preservation of the pretarsal portion of the orbicularis oculi muscle, thus minimizing the risk of postoperative lower eyelid malposition. Meticulous hemostasis is achieved with bipolar cautery throughout the procedure.
 Figure 1 (A) The incision is 2 mm inferior to the lower lid margin and extends from the lower punctum medially to a position 6 mm lateral to the lateral canthus. Following the skin incision, fine curved scissors are used to dissect through the orbicularis muscle at the lateral aspect of the incision, thus exposing the orbital septum. (B) Outwardly beveled blunt scissors are introduced posterior to the muscle at the lateral aspect of the incision and, with spreading motions of the blunt scissors, the skin-muscle flap is effectively elevated off the orbital septum along an avascular plane to the level of the inferior orbital rim inferiorly and the incision superiorly.
Figure 1 (A) The incision is 2 mm inferior to the lower lid margin and extends from the lower punctum medially to a position 6 mm lateral to the lateral canthus. Following the skin incision, fine curved scissors are used to dissect through the orbicularis muscle at the lateral aspect of the incision, thus exposing the orbital septum. (B) Outwardly beveled blunt scissors are introduced posterior to the muscle at the lateral aspect of the incision and, with spreading motions of the blunt scissors, the skin-muscle flap is effectively elevated off the orbital septum along an avascular plane to the level of the inferior orbital rim inferiorly and the incision superiorly.

Access to the orbital fat compartments is obtained through small, selected openings of the orbital septum. Gentle palpation of the globe results in herniation of orbital fat through the aforementioned openings of the orbital septum. Bipolar cautery is used to cauterize the fat pad before excision; prior to cauterization, local anesthetic is infiltrated in the fat pocket to minimize pain. This procedure is performed for the lateral, middle, and medial fat pockets. Gentle palpation of the globe following resection of orbital fat allows reassessment of orbital fat. A conservative approach to fat resection is maintained to avoid the creation of a sunken appearance. On completion of fat resection, the skin-muscle flap is repositioned. If mildly sedated, the patient is asked to open his mouth and look up; this maneuver allows maximal separation of wound edges and subsequent conservative resection of skin and muscle. If the patient is completely sedated, single-finger pressure at the inferomedial portion of the melolabial mound will create the same maximal stretch effect. Following this, an inferiorly directed segmental cut is made at the lateral canthus to determine the amount of excess skin to excise (Fig. 2A). A tacking suture is placed to maintain the position of the skin-muscle flap; eyelid scissors are then used to excise the overlapping skin (Fig. 2B). If orbicularis oculi muscle hypertrophy is evident, a 1- to 2-mm strip of muscle is resected to prevent overlapping of muscle and ridge formation with closure of the subciliary incision (Fig. 2C). Conservative resection of both skin and muscle decreases the incidence of postoperative lower eyelid malposition. In addition, suspension of the orbicularis oculi muscle to the periosteum of the lateral orbital rim assists in maintaining proper lid position (Fig. 3A and 3B). If there is evidence of festoons or malar mounds, an extended lower lid blepharoplasty is performed inferior to the infraorbital rim; the redundant orbicularis oculi muscle or malar mounds, or both, are addressed by advancing the entire skin-muscle flap and suborbicularis oculi fat (SOOF) unit superiolaterally. Following muscle suspension, the subciliary incision is closed with 7-0 blue polypropylene suture at the lateral canthus; the remainder of the incision is closed with 6-0 mild chromic suture (Fig. 4A and 4B).

Figure 3 (A) Suspension of the orbicularis oculimuscle to the periosteum of the lateral orbital rim at the tuberclewith 5-0 polyglyconate (Maxon) maintains proper lid position. (B) Superolateral advancement of the skin-muscle flap.

Figure 4 (A) Preoperative and (B) postoperative photographs following transcutaneous lower blepharoplasty in the male patient; of note, upper blepharoplasty was performed at the same time on this patient.
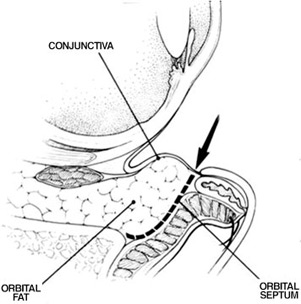
Figure 5 The preseptal approach to the transconjunctival blepharoplasty utilizes an incision located inferior to the tarsus and not deep to the inferior fornix, allowing a more anterior to posterior approach to the fat pockets. 8
Compared with the transconjunctival approach, the transcutaneous approach affords the ability to correct true vertical excess of lower lid skin and orbicularis oculi hypertrophy. Therefore, the senior author most often uses the transcutaneous approach in lower lid blepharoplasty. However, there are specific indications for the transconjunctival approach.9 For example, young patients with excellent elasticity, presence of hereditary pseudoherniation of orbital fat, and no evidence of skin excess are ideally suited for the transconjunctival approach. In addition, patients with Fitzpatrick skin types V and VI may benefit from the transconjunctival approach as the transcutaneous lower lid blepharoplasty scar may depigment in these patients. Finally, the transconjunctival approach results in transection and release of the inferior retractor muscles, allowing a temporary rise in the lower lid position. This fact makes the transconjunctival approach an ideal procedure for secondary lower lid blepharoplasty.10 During transconjunctival blepharoplasty, the senior author utilizes a preseptal approach through an incision located inferior to the tarsus and not deep in the inferior fornix; this allows a more anterior to posterior approach to the fat pockets (Fig. 5).11
ADJUNCTIVE PROCEDURES
Fat Transposition
Many methods have been utilized to efface the tear trough deformity, including fat grafts, injections with fat or injectable fillers,12 and alloplastic implants.13 Also, transposition of pedicled orbital fat into a subperiosteal pocket over the orbital rim has been performed by both transconjunctival and transcutaneous approaches.14 The senior author performs fat transposition by a transcutaneous approach in conjunction with lower lid blepharoplasty in patients who demonstrate a tear trough deformity. Preoperatively, the tear trough deformity is marked out with a pen. Lower lid blepharoplasty with
extension below the infraorbital rim is performed. Once the orbital fat from the medial pocket is isolated from the orbital septum, it is transposed over the orbital rim and positioned into a pocket posterior to the orbicularis oculi muscle and anterior to the periosteum to efface the tear trough deformity. The transposed orbital fat is then secured to the periosteum using interrupted 6-0 polyglycolic acid (Dexon) sutures (Fig. 6). The contour of the orbital fat is then softened with the use of bipolar cautery. Subsequently, the lower lid blepharoplasty is completed as previously described (Fig. 7).

Figure 6 (A) Fat transposition. A pocket is created posterior to the orbicularis oculi muscle but anterior to the periosteum. (B) The medial fat pocket is released from the surrounding orbital septum and subsequently sutured over the infraorbital rim into the previously made pocket with 6-0 polyglycolic acid (Dexon).
Lateral Canthoplasty
Lower lid malposition may be related to retraction or ectropion. In an effort to minimize postoperative lower lid malposition during lower lid blepharoplasty, the senior author routinely preserves the pretarsal orbicularis oculi muscle, resects skin and muscle in a conservative fashion, and suspends the orbicularis oculi muscle to the periosteum of the lateral orbital rim. In addition to the aforementioned intraoperative maneuvers, preoperative evaluation of lower eyelid tone and position is
essential in decreasing the incidence of postoperative lower lid malposition. If the lower eyelid demonstrates malposition or poor tone preoperatively, a lateral canthoplasty is performed in conjunction with lower lid blepharoplasty. Following lateral canthotomy and inferior cantholysis, the tarsus is dissected from the skin, muscle, and conjunctiva. The tarsal strip is then attached using permanent suture to the medial aspect of the lateral orbital rim periosteum in a posterosuperior position.
Then the appropriate amount of lower lid is excised (Fig. 8).
Skin Resurfacing
Lower lid blepharoplasty cannot effectively efface periorbital rhytids. Therefore, skin resurfacing can be performed
in conjunction with lower lid blepharoplasty. However, vertical contracture of the lower eyelid may occur following blepharoplasty and result in lower lid malposition. Skin resurfacing may also result in skin tightening of the lower eyelid and subsequent ectropion. Therefore, it is essential to evaluate both lid position and lid support prior to performing skin resurfacing in conjunction with lower lid blepharoplasty and consider canthoplasty if the lower eyelid demonstrates malposition or poor support, or both. Ideal candidates for skin resurfacing of the lower eyelid include patients with Fitzpatrick skin types I to III. The senior author prefers an 88% phenol peel or CO2 laser resurfacing for the lower eyelid skin. These skin resurfacing modalities are safely performed in conjunction with the transcutaneous blepharoplasty. However,
as previously discussed, one should consider performing a lateral canthoplasty if the lower eyelid demonstrates malposition or poor support. Typically, the senior author combines a variety of resurfacing modalities, such as an 88% phenol peel of the lower eyelid region and CO2 laser resurfacing of the perioral region; a 35% trichloroacetic acid (TCA) peel of the entire face performed in conjunction with the aforementioned regional resurfacing techniques will blend these regions and provide a well-balanced, harmonious result.

Figure 7 (A) Preoperative and (B) postoperative photographs demonstrating effacement of the tear trough deformity following transcutaneous lower lid blepharoplasty with fat transposition.
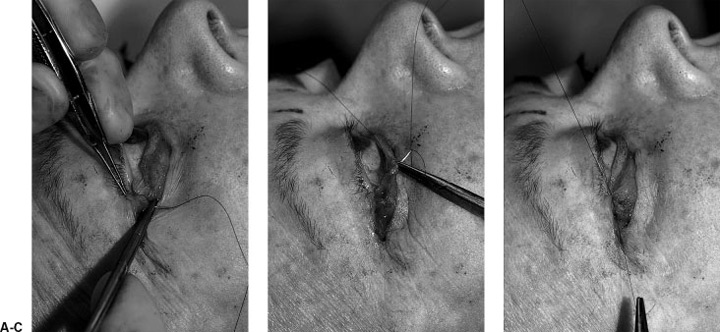
Figure 8 Lateral canthoplasty. Following lateral canthotomy and lateral cantholysis, the tarsus is separated anteriorly from the skin and orbicularis oculi muscle and posterior Ly from the conjunctiva. A 5-0 polypropylene (Prolene, usually clear) is passed through (A) the periosteum of the medial aspect of the lateral orbital rim in a posterosuperior position and (B) the tarsus to (C) improve lid position and support.
CONCLUSIONS
Rejuvenation of the lower eyelid complex in the male patient requires proper preoperative evaluation. In doing so, the facial plastic surgeon can select the proper treatment modality. Blepharoplasty performed in conjunction with fat transposition, canthoplasty, and/or skin resurfacing can result in a less tired, more youthful appearance of the lower eyelid complex.
ACKNOWLEDGMENTS
The authors would like to acknowledge Nancy A. Rothrock for her assistance in the preparation of digital images used in this article.
REFERENCES
- Verity DH, Collin JR. Eyelid reconstruction: state of the art. Curr Opin Otolaryngol Head Neck Surg 2004;12:344–348
- Friedman O. Changes associated with the aging face. Facial Plast Surg Clin North Am 2005;13:371–380
- Rankin BS, Arden RC, Crumley AL. Lower eyelid blepharoplasty. In: Papel ID, ed. Facial Plastic and Reconstructive Surgery 2nd ed. New York: Thieme MedicalPublishers; 2002:196–207
- Bernardi C, Dura S, Amata PL. Treatment of orbicularis oculi muscle hypertrophy in lower lid blepharoplasty. Aesthetic Plast Surg 1998;22:349–351
- Mendelson BC, Muzaffar AR, Adams WP. Surgical anatomy of the midcheek and malar mounds. Plast Reconstr Surg 2002;110:885–896
- Kawamoto HK, Bradley JP. The tear ”TROUF” procedure: transconjunctival repositioning of orbital unipedicled fat. Plast Reconstr Surg 2003;112:1903–1907
- Moses JL. Blepharoplasty: cosmetic and functional. In: McCord CD, Tantenbaum M, Nunery W, eds. Oculoplastic Surgery 3rd ed. New York: Raven Press; 1995:285–318
- Perkins SW, Latorre RC. Blepharoplasty. In: Romo T, Millman AL, eds. Aesthetic Facial Plastic Surgery. New York: Thieme Medical Publishers; 2000:262–287
- Perkins SW. Transconjunctival lower lid blepharoplasty. Facial Plast Surg Clin North Am 1995;3:175–187
- Fedok FG, Perkins SW. Transconjunctival blepharoplasty. Facial Plast Surg 1996;12:185–195
- Perkins SW, Dyer WK 2nd, Simo F. Transconjunctival approach to lower eyelid blepharoplasty: experience, indications, and techniques in 300 patients. Arch Otolaryngol Head Neck Surg 1994;120:172–177
- Kane MA. Treatment of tear trough deformity and lower lid bowing with injectable hyaluronic acid. Aesthetic Plast Surg 2005;29:363–367
- Flowers RS. Tear trough implants for correction of tear trough deformity. Clin Plast Surg 1993;20:403–415
- Goldberg RA. Transconjunctival orbital fat repositioning: transposition of orbital fat pedicles into a subperiosteal pocket. Plast Reconstr Surg 2000;105:743–74

